Do No Harm: Osheroff v. Chestnut Lodge and the Future of Psychiatry
The Osheroff case made medicine an inappropriate God of psychiatry.
The protagonist in Do No Harm is not likely a name you would know, Dr. Raphael Osheroff. Ray was a physician, a nephrologist. He passed away almost a decade ago. At the time of his death, he was an ordinary man, who for the past quarter century led a quiet but complicated life. Many who knew Ray during this period would have been surprised to discover that Ray had played a seminal role in shaping the course of American psychiatry for the past 40 years. Not because he made a significant scientific contribution. Not because he discovered a novel drug. Not because he treated a famous patient. But because of the legal dispute he had with an exclusive private psychiatric hospital, Chestnut Lodge, the hospital made famous by Joanne Greenberg's bestselling book and Roger Corman's 1977 film of the same name, I Never Promised You a Rose Garden.
Ray was “treated” exclusively with psychoanalysis, which not only failed to relieve his depression but made it worse. Much worse. His frequent requests for medicine were refused on the grounds that “he would need every neuron” to fight his disease.
What makes this story so captivating is that Ray Osheroff sued Chestnut Lodge for malpractice not because of what they did but because of what they refused to do: prescribe medicine to treat his “agitated depression” which was the DSM-2 diagnosis he received at the time.1 During his seven-month residency at the Lodge, as it was commonly known, Ray was “treated” exclusively with psychoanalysis, which not only failed to relieve his depression but made it worse. Much worse. His frequent requests for medicine were refused on the grounds that “he would need every neuron” to fight his disease.2
The harm done was because of what was not done. As Harvard Law School Professor Alan Stone explained at the time, “the central irony of the case was that Chestnut Lodge was being sued for malpractice for not treating a patient with drugs, but in Massachusetts, Colorado, and other states, judges had ruled that patients have the right to refuse drug treatment, and doctors were being forced to treat them in a way Osheroff claims was negligent.”3
He looked like a skid row derelict with long unkempt hair, baggy clothes, slippers that were made out of paper, belt holding pants up. He was unkempt, unwashed … would not, could not sit still. Could not stop pacing.
Over the course of several months, not only his psychological but also his physical symptoms became so dire that his dear friend and personal attorney, Arnold Westerman, who had to force his way into the Lodge to visit his client, could hardly believe his eyes: “He looked like a skid row derelict with long unkempt hair, baggy clothes, slippers that were made out of paper, belt holding pants up. He was unkempt, unwashed … would not, could not sit still. Could not stop pacing.”4
Ray's feet were a blistered and bloody mess from pacing as many as 16 hours a day. His toes had turned black. They were so bad he required regular visits with Dr. Edward Ganny, a podiatrist who had devoted hours to treating the blisters, calluses, and corns to prevent a dangerous infection. His weight had plummeted more than 40 pounds. His fine motor skills had atrophied to the point at which he struggled to handle a fork and knife forcing him to “eat like an animal.” The damage to his back and hips he sustained from miles of daily pacing would later require physical therapy to address a refractory case of bursitis. He would likewise require weeks of occupational therapy to regain the fine motor skills he needed to navigate a dinner table and use a pen to sign his signature.5
But it was not only Ray's physical and emotional state that concerned Arnold Westerman. He was also worried about the personal and professional turmoil that was engulfing his client's life beyond the walls of his locked ward at the Lodge and which, in his current condition, Ray was powerless to address. A once fastidious man who wore bespoke suits, drove expensive cars, and frequented the region's most fashionable establishments, Ray had become a pale shade of his former self – not only oblivious to his appearance but also lacking the energy and focus to address his crumbling personal and professional affairs which, taken together, became the motivating force behind his suit against the Lodge.
A “Landmark” Case
At its core Osheroff v. Chestnut Lodge was a legal dispute between an aggrieved patient seeking justice and a hospital and two physicians claiming they had done nothing wrong. But if that were all it was, it would have hardly elicited the interest and passion, let alone the extraordinary effort and time commitment of one the greatest civil rights attorney of the past century along with some of the most eminent psychiatrists of their generation – many of whom dropped what they were doing and gave hundreds of hours of their precious time to the case – scrutinizing medical records, devoting hours to being deposed by opposing counsel; and testifying under oath, thereby subjecting themselves to brutal cross examination.
When Professor Stone called Osheroff v. Chestnut Lodge a landmark case, he was not exaggerating. For both the attorneys and their A-list expert witnesses, a great deal more was on trial than the fate of an aggrieved individual and a famous psychiatric hospital that catered to the wealthy. As Dr. Thomas Gutheil, among the nation's most acclaimed forensic psychiatrists for the past two generations (and an expert witness during the Osheroff case), explained to me over lunch earlier this year, “The Osheroff case made medicine an inappropriate God of psychiatry.”6
Why Osheroff v. Chestnut Lodge Still Matters
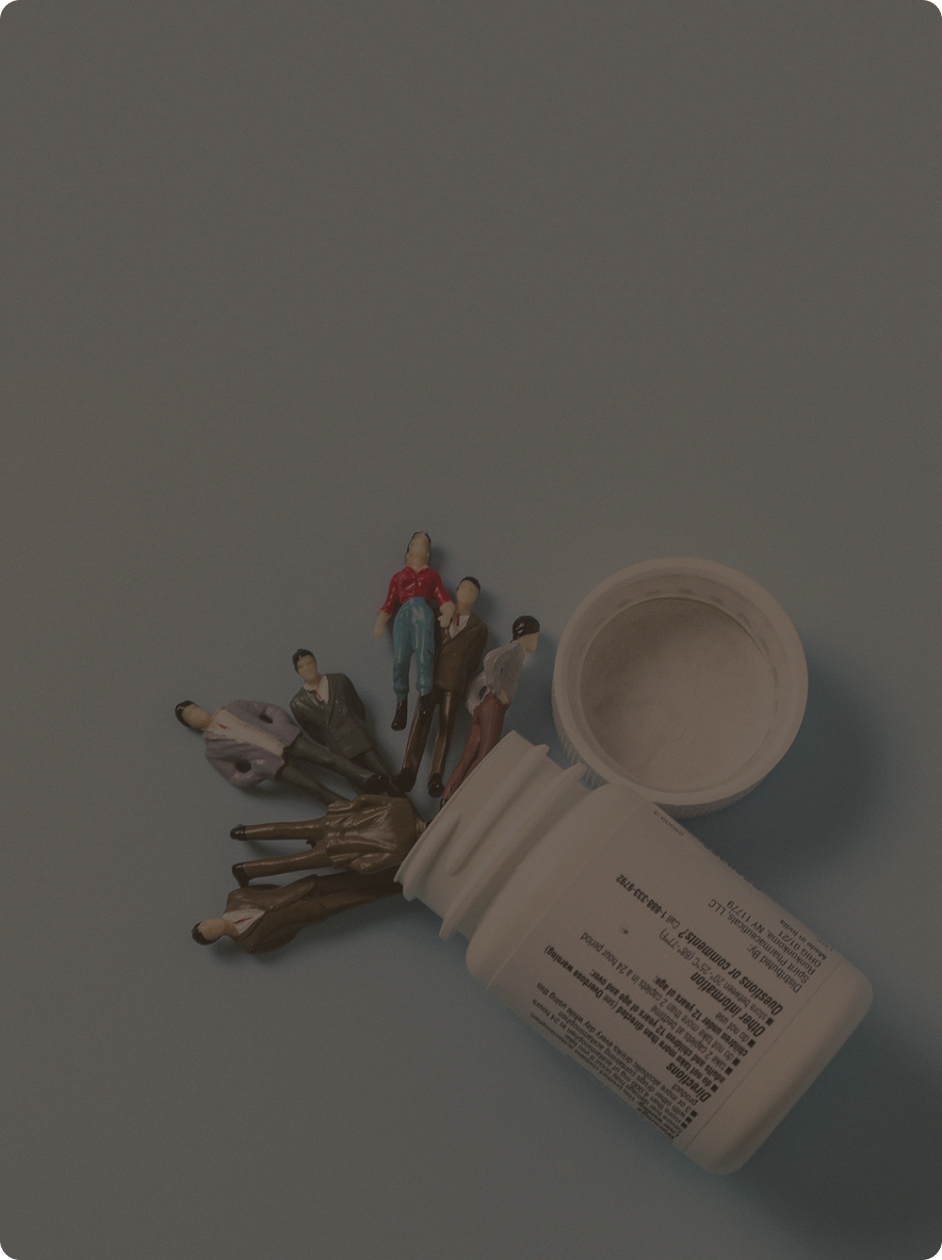
In 1987 the year the Osheroff case settled, Prozac (fluoxetine) became the first US Food and Drug Administration (FDA)-approved selective serotonin reuptake inhibitor (SSRI). It is now more than 35 years since the first prescription of an SSRI was filled in the United States. Over this period Americans have swallowed billions of these tablets and capsules. While simultaneously (and, in part, because of the relatively inexpensive cost to treat mental illness with drugs compared to more costly psychosocial interventions), the prospects of those with mental illness have declined precipitously over this same period.
As historian Andrew Scull explains in his brilliant new book, Desperate Remedies: Psychiatry's Turbulent Quest to Cure Mental Illness, “From the patient's point of view, all these developments have occurred alongside the collapse of public psychiatry and the consignment of many of the mentally ill to the squalor of the streets and the terrors of American jails. For those retaining any lingering disposition to embrace a narrative of psychiatric progress, there is the brutal reality that those suffering from serious mental illness have a lifespan of 20 to 30 years less on average than the rest of us – and this is a mortality gap, moreover, that is increasing, not diminishing.”7
I succeeded in getting lots of really cool papers published by cool scientists at fairly large cost − I think $20 billion – [but] I don't think we moved the needle in reducing suicide, reducing hospitalizations, improving recovery for the tens of millions of people who have mental illness.
Scull's assessment is hardly the screed of an anti-psychiatrist. A virtually identical cri de cœur recently echoed from the nation's temple of institutional psychiatry. Describing what he accomplished during his 13-year tenure as “America's psychiatrist” former National Institute of Mental Health (NIMH) Director, Thomas Insel, confesses in his recent and much discussed book, Healing: Our Path From Mental Illness to Mental Health, “I succeeded in getting lots of really cool papers published by cool scientists at fairly large cost − I think $20 billion – [but] I don't think we moved the needle in reducing suicide, reducing hospitalizations, improving recovery for the tens of millions of people who have mental illness.”8
To address our mounting mental healthcare crisis – one that transcends race, class, gender, and identities of all stripes – we need to radically reconceptualize how we respond to and address the needs of those suffering from these invisible wounds. We also need to reconsider the centrality of pharmaceutical solutions to the exclusion of other psychosocial interventions. But to do so effectively, we need first to understand how we arrived at this crisis point. I believe the best way to achieve this understanding is through a well-written, richly nuanced, engaging story. One that captivates readers and audiences; inspires them to think differently and to imagine, if only for a brief moment, that Ray's story could be their story or the story of someone they love.
1 Raphael Osheroff Admission Note, Chestnut Lodge, January 2. 1979.
2 Osheroff v. Chestnut Lodge, Maryland HCA No. 82-262, December 5, 1983.
3 Alan Stone, as quoted in Osheroff v. Chestnut Lodge, International Medical News Group, August 1986.
5 Osheroff v. Chestnut Lodge, Maryland HCA No. 82-262, Statement of Fact.
6 Author interview with Dr. Thomas Gutheil, Fugakyu,1280 Beacon St, Brookline, MA 02446, April 2, 2022.
7 Andrew Scull, Desperate Remedies: Psychiatry’s Turbulent Quest to Cure Mental Illness, Cambridge: The Belknap Press of Harvard University, 2022, p.
8 Thomas Insel, Healing: Our Path From Mental Illness to Mental Health, New York: Penguin Press, 2022.